Hey, my name is Judy and I was diagnosed with triple negative breast cancer while on maternity leave with my third child. It was March 2019, and at the end of the day I always take my bra off and give my tatas a little massage. I found a small lump that felt like a Skittle. I had my husband feel it and he thought it was unusual as well. I was 9 months into my maternity leave so I figured maybe it was hormones balancing out but my mind was racing that night. I got in to my doctor’s office 2 days later and saw my friend who is a nurse, she felt it and had the doctor in the office that day feel it as well. I was expecting them to give me all the right words to diffuse my concern. I was hoping they would say that it felt totally normal but that we would do tests to be sure, or better yet, to stop my worrying. This was not the case. They had concerned faces, and I got the requisition for an ultrasound and biopsy. I move through these steps but the thoughts of “why me, why this, and why now” were toxic and overwhelming. That and a two month wait for results were perhaps the hardest of all the days with no direction, no diagnosis and no plan.

We had a road trip to Disney World with our entire family planned during that month. It kept me busy but my mind was still very much consumed with wonder. While on vacation I was very much living in a “what if?” state of mind. It was somewhat of a blessing because it forced me to go on rides at Disney I would have never gone on with my oldest. My mind frame each day was “what if this is my last time here, or last time on a family vacation…I’m going on the ride, I’m buying any souvenir my kids want, or I want!” It was good in a way because we did everything and we went all out! It will certainly be a trip we will never forget. But hard because so much of the risk taking and moment loving came from a place of worry and fear. It had a sobering way of making me seize the moments and ferociously love my family.
My doctor called while we were on vacation (about 2 weeks after the biopsy). She said the results needed a second opinion. I had a complete meltdown, it lasted about an hour. I called a friend from home who works in the medical field and she shed some light on why it might need a second opinion and she totally settled me down. About a week after we got home my doctor called me into her office. That’s the first time that has ever happened and I knew it couldn’t be good. When I arrived the nurse (my friend) came out and asked if my husband was coming in, it was like a rush of adrenaline hit me, I knew why she was asking if he’d be there….he wasn’t, he was returning later because he was out of town for work. A few minutes later they called me into the office. I could tell they had been crying, both my doctor and nurse are friends. “You have invasive ductal carcinoma” is what she said. The word “invasive” seemed so scary to me at the time. I had a million questions flood my mind and knew they couldn’t be answered then but I started babbling them off anyway. “Am I going to die? How will I tell my oldest daughter? I don’t want to see my parents cry…what’s going to happen? What does this mean?” Then I cried. Then I drove home and my parents were there waiting for me. I went for a drive with my mom, it was like a pep talk. “We got this, we will do whatever it takes, it’s ok”. When we got back home my husband was there he gave me a hug and I could tell he’d been crying. Then I felt like the adrenaline had left my body and I could finally breathe. But then I wanted to search the internet “invasive ductal carcinoma” but I did my best to leave that to my husband. At this stage the words felt foreign, the diagnosis didn’t seem real and the next steps felt like someone else’s path and not my own.

I updated my friends and family with my news. Each time I said it out loud it became a little more real. And then in a moment of vulnerability to this new reality, I started sharing my story on my Instagram account and the support was overwhelming. It was so helpful. It kept me focused. If I was feeling down or sad I’d open my messages and I would read encouraging words from family, friends and even old friends I’d lost touch with. It was incredible. It was a big and hard step as a normally quite private person but I quickly realized what an important role sharing your story is when it comes to the acceptance, battle and healing from this disease. Then my best friend who lives in Nashville shared the Tata to Cancer site with me. I felt like I connected with so many of the women on the blog. It was the best thing for me to read. No more searching the internet and reading horror stories, I read about these brave women and their journeys. I started following many of them online and it encouraged me to do the same and share my story.

My husband and I told our oldest daughter I had breast cancer together. We said “I have a small lump in one of my breast (pointed to it), it’s cancer. I’m going to get medicine that may make me sick, and then I will have surgery to cut the cancer out. But because I take care of my body the rest of me is still very healthy and I am going to fight this.” She said “you are so strong Mommy, you will fight this and win, I will help you”. She gave me the best hug and I cried and she told me “it will be ok”. I have never felt so ready to fight in my life. In that single moment, I saw my 7 year old girl as a young woman, a supportive, brave, empathetic young woman and I was both sad for what we were about to go through as a family but so proud that she was mine.
An appointment with my surgeon was scheduled for 3 weeks later. 3 MORE WEEKS of waiting. The waiting was incredibly hard. I could no longer hold back from searching online. It was the worst thing for me. I would read awful stories and negative comments…it felt never ending. When I would stop I would be crying and my husband had to talk me through everything we knew about MY situation, not everyone else’s situation online. It was hard.

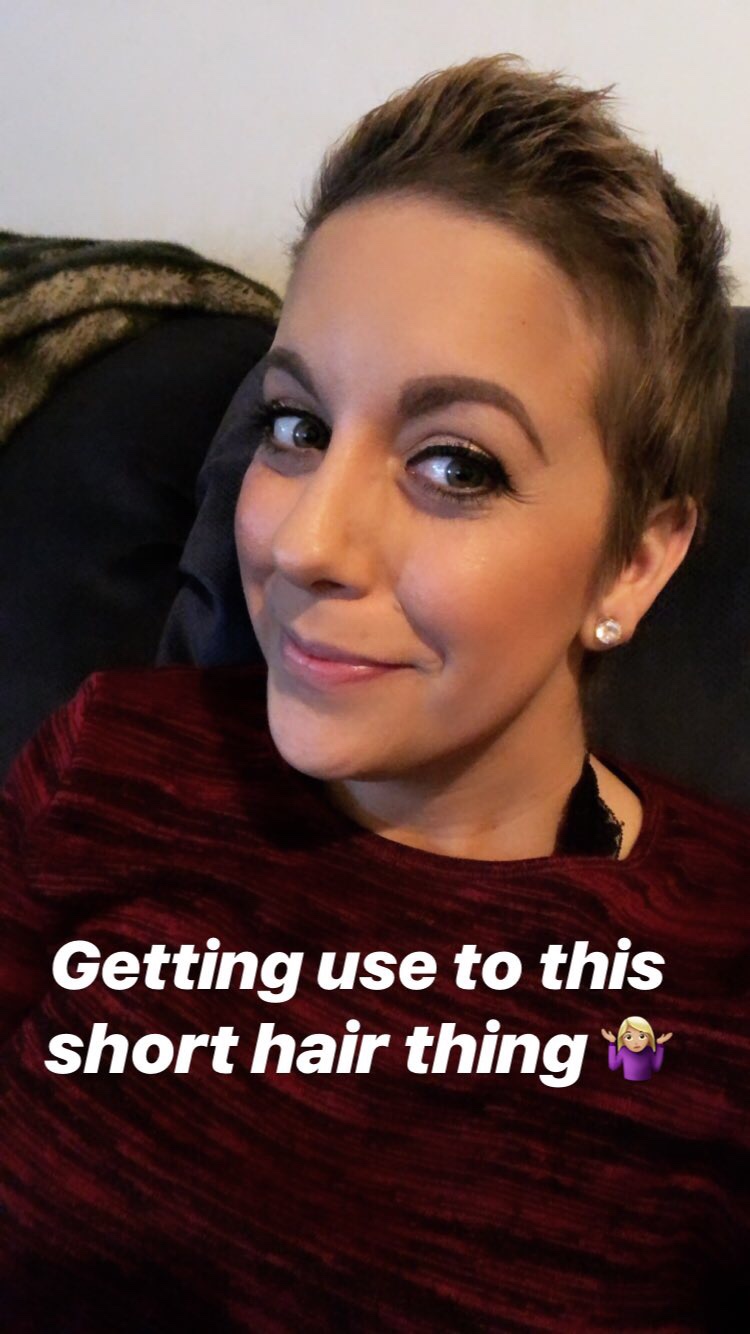
I met my surgeon and I ended up needing another biopsy which delayed the process a bit longer. But after that and a few more mammograms I was so over people telling me what was going to happen to my body I went and got my hair cut short. This was very empowering. I finally felt in control. Then a couple weeks later I went even shorter. I was finding it comforting taking control and playing with new styles. My hairdresser was amazing, she and her husband and brand new baby welcomed me into their home at any time just to help me through that difficult stage. It was so good for me. My surgeon told me I’d lose my hair, there was no doubt it would fall out, so I wasn’t worried about doing it too soon.
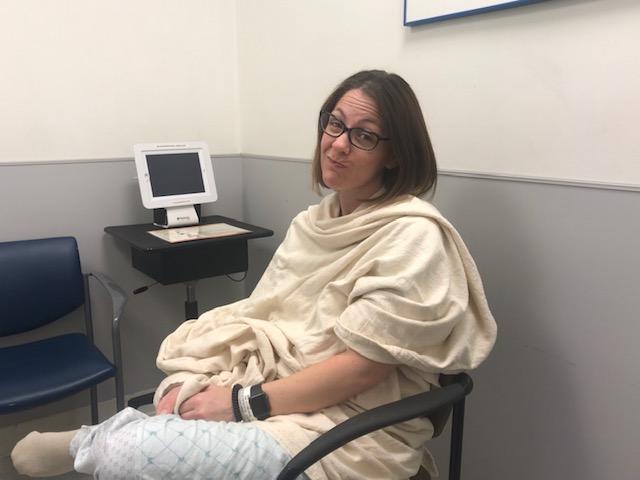
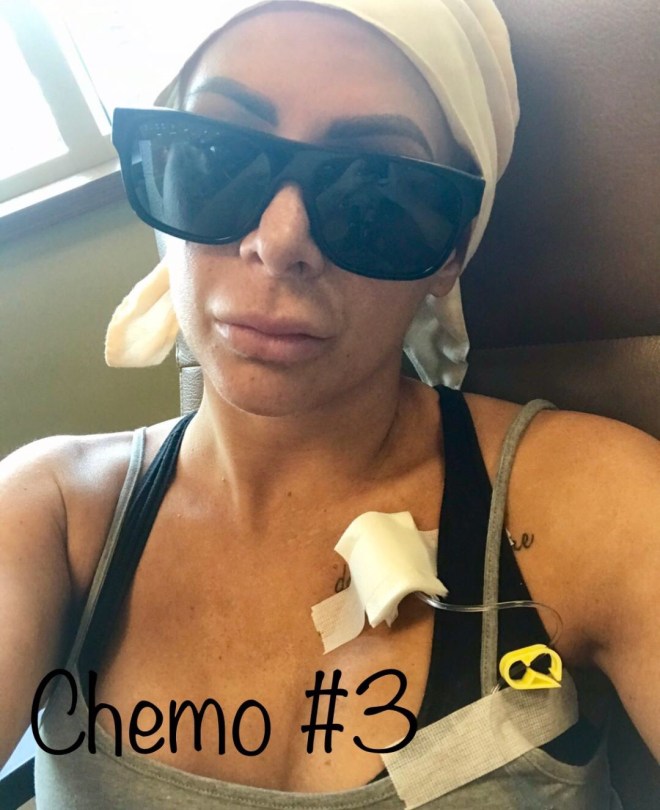
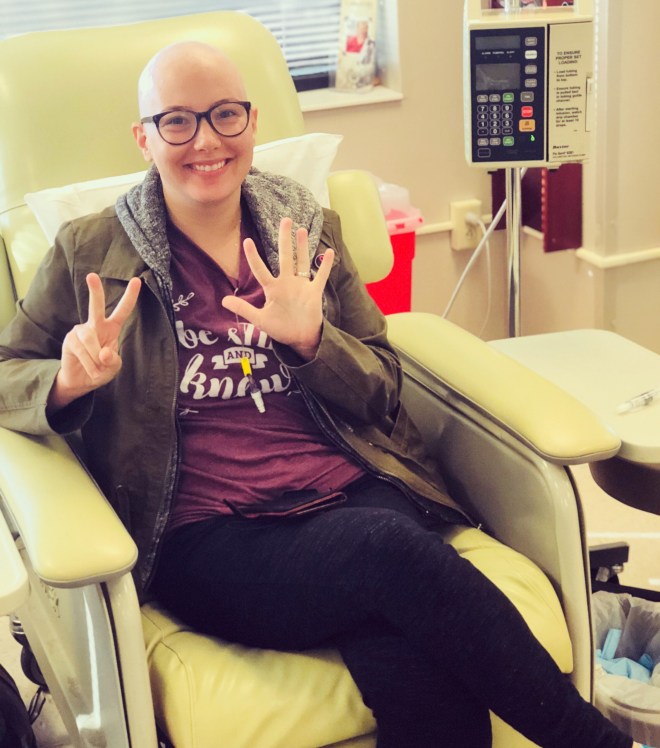
I had my first round of chemo 3.5 months after finding my lump. As nervous as I was I was ready, I wanted to start this fight and move on. I had chemo on a Monday afternoon and by that evening I was incredibly nauseous and exhausted. This lasted for 3 days. Then from day 4-5 I was able to leave the house for an hour and come home and have a two hour nap. By day 6 I was feeling like myself again. I was so happy to eat solid food and feel like myself. I knew if this is what it was like I could handle it. I could do 6 days of feeling like crap and 15 days of myself for a few months.
I had docetaxel for my 4th and 5th round (#6 to come this month). At first I thought this is great, I was sore but it was manageable. But it lingered for days. I was sore, achy, had nose bleeds, headaches, bruising, pain in my fingers and joints and I couldn’t taste anything. I wasn’t myself after this and that made things hard for me. But I only have 1 round left and then surgery and radiation. I’m over the half way point of chemo, knowing that helps.

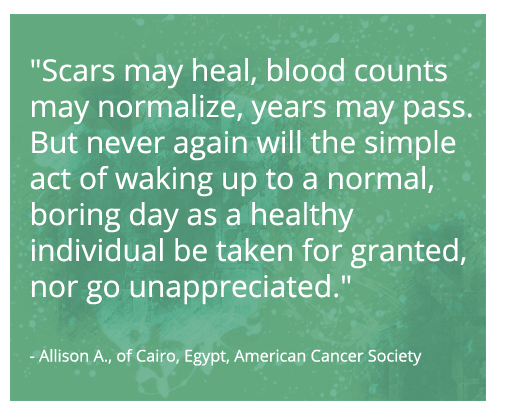
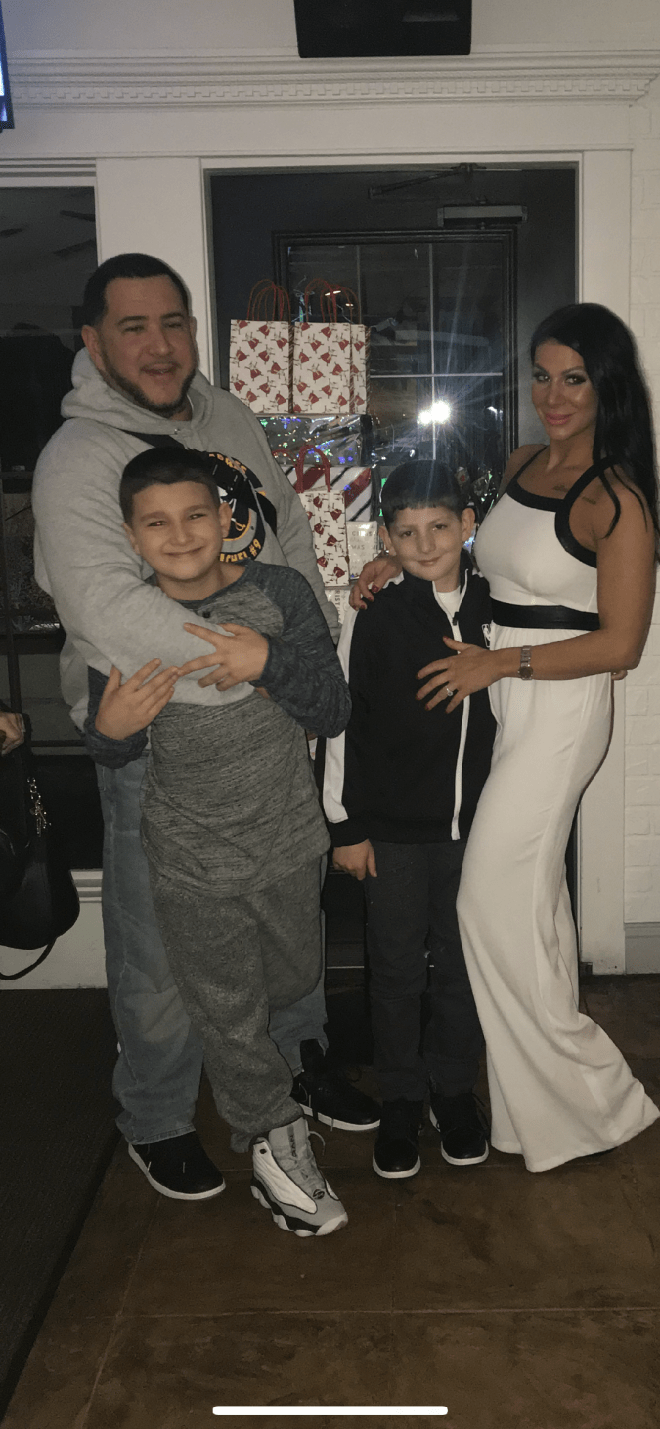
My family, friends and community have been my inspiration. They have been incredibly supportive. My family has received cards, food, gift cards, money, babysitting, visits, gift baskets and more. This journey has brought us closer to our family, friends and community. I have my down days and during those times I read through the cards and emails people have sent and it brings me back up. My husband has been AMAZING. He’s always one step ahead of me, lifting me up, bringing me a treat or picking up the kids early and taking them out when he knows I’m just too tired. He makes staying positive easier. The kids make it easier. Reading about other women and their journeys make it easier. I hope that sharing my story can help at least one person or a family member get through a tough moment. xo









 From my mammogram back in May I was sent back for a recheck, then had ultrasound guided biopsy and then also a steristatic biopsy. Following both of those positive findings of invasive lobular carcinoma, I was also sent for an MRI which confirmed those two spots as well as found two other very small spots.
From my mammogram back in May I was sent back for a recheck, then had ultrasound guided biopsy and then also a steristatic biopsy. Following both of those positive findings of invasive lobular carcinoma, I was also sent for an MRI which confirmed those two spots as well as found two other very small spots.



































 This news from him was like a ton of bricks hitting my husband and me. All I could think about was my 5-year-old son and what we were going to do. So we go about the day have the biopsies and the nurse tells us she will call us at 3pm on Friday. The nurse calls us on Friday and confirms that diagnosis, Stage II, Invasive Ductal Carcinoma. I have to tell you the next hour was a complete whirlwind. She scheduled my appointment with the breast surgeon for first thing Monday morning. Oh and by the way this official diagnosis was the day before my wedding anniversary. My husband and I decided to put it all behind us and just have a great weekend without thinking about the diagnosis….like that happened.
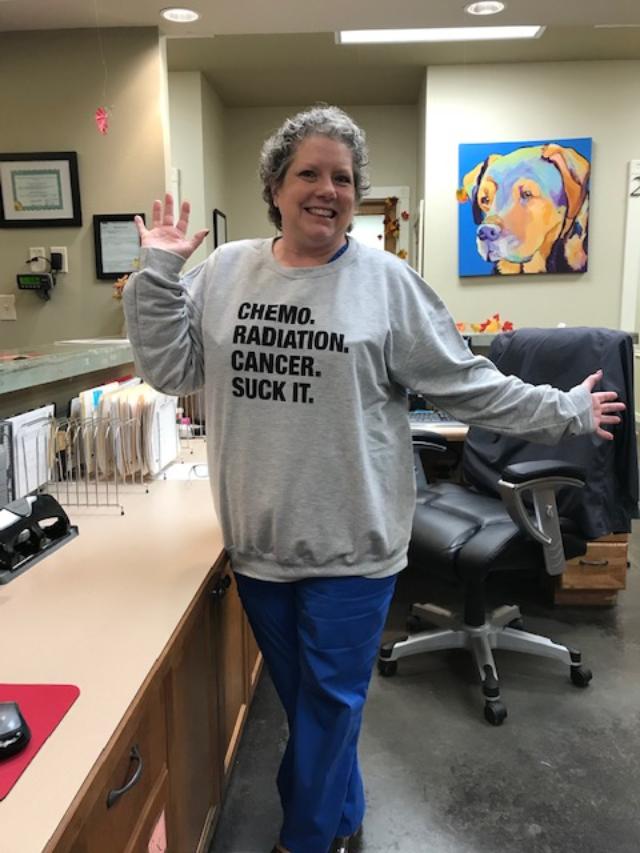
This news from him was like a ton of bricks hitting my husband and me. All I could think about was my 5-year-old son and what we were going to do. So we go about the day have the biopsies and the nurse tells us she will call us at 3pm on Friday. The nurse calls us on Friday and confirms that diagnosis, Stage II, Invasive Ductal Carcinoma. I have to tell you the next hour was a complete whirlwind. She scheduled my appointment with the breast surgeon for first thing Monday morning. Oh and by the way this official diagnosis was the day before my wedding anniversary. My husband and I decided to put it all behind us and just have a great weekend without thinking about the diagnosis….like that happened. my decision at my first appointment to have a double mastectomy because I didn’t want to worry about it coming back in my other breast. So I had chemo, last one was in July, I had talked my breast surgeon into doing my surgery in August because my blood numbers had been good all through the chemo. I didn’t have any issues during chemo except for neuropathy. I was scheduled to have my surgery and I was having my pre surgery appointment, four days before my surgery, with my plastic surgeon and he says I am not doing your surgery, it’s too close to the end of your chemo. I get to my car and call my breast surgeon, surprisingly she answers. I tell her what’s going on and she then calls me 10 minutes later letting me know to be back there at 7:30am in the morning and another doctor would perform my surgery on Tuesday. Don’t worry everything will be ok. Again I am freaked out but I can handle this. So I meet with the new doctor and he is amazing. We go to the hospital Tuesday amped up and ready to get this part over with, I am a pretty type A person so this whole process has been hard for me to not be able to control. After the surgery we got word that my margins came back clear and so did my lymph nodes. This might have been the best news I ever heard. I told myself I was only going to be off work for two weeks…and I was. I went back to work after 9 work days, still had 3 tentacles (drains). I think my doctors gave up telling me what to do, I showered after three days with my drains and all. I drove after a week. I was not going to let this dictate my life any more than it had. Yes, maybe I should have listened to the doctors, but it ended up okay. I healed well, started with the expanders or as I called them the fluff and fills every week. I was such a planner that in October I told my doctor when I wanted to do the exchange surgery and we got to an agreement. I had my exchange surgery on Dec. 22. Maybe not a great idea to do a few days before Christmas but I wanted it done before the New Year.
my decision at my first appointment to have a double mastectomy because I didn’t want to worry about it coming back in my other breast. So I had chemo, last one was in July, I had talked my breast surgeon into doing my surgery in August because my blood numbers had been good all through the chemo. I didn’t have any issues during chemo except for neuropathy. I was scheduled to have my surgery and I was having my pre surgery appointment, four days before my surgery, with my plastic surgeon and he says I am not doing your surgery, it’s too close to the end of your chemo. I get to my car and call my breast surgeon, surprisingly she answers. I tell her what’s going on and she then calls me 10 minutes later letting me know to be back there at 7:30am in the morning and another doctor would perform my surgery on Tuesday. Don’t worry everything will be ok. Again I am freaked out but I can handle this. So I meet with the new doctor and he is amazing. We go to the hospital Tuesday amped up and ready to get this part over with, I am a pretty type A person so this whole process has been hard for me to not be able to control. After the surgery we got word that my margins came back clear and so did my lymph nodes. This might have been the best news I ever heard. I told myself I was only going to be off work for two weeks…and I was. I went back to work after 9 work days, still had 3 tentacles (drains). I think my doctors gave up telling me what to do, I showered after three days with my drains and all. I drove after a week. I was not going to let this dictate my life any more than it had. Yes, maybe I should have listened to the doctors, but it ended up okay. I healed well, started with the expanders or as I called them the fluff and fills every week. I was such a planner that in October I told my doctor when I wanted to do the exchange surgery and we got to an agreement. I had my exchange surgery on Dec. 22. Maybe not a great idea to do a few days before Christmas but I wanted it done before the New Year.
 but still is amazing and supportive, my family that sticks my me and offers to help whenever I need it and all of my friends. I truly could not have done this without the support system I have, it’s overwhelming but to know people are out there loving and supporting me and looking at me as an example makes me want to keep pushing on. Love you all and thanks for reading!
but still is amazing and supportive, my family that sticks my me and offers to help whenever I need it and all of my friends. I truly could not have done this without the support system I have, it’s overwhelming but to know people are out there loving and supporting me and looking at me as an example makes me want to keep pushing on. Love you all and thanks for reading!

















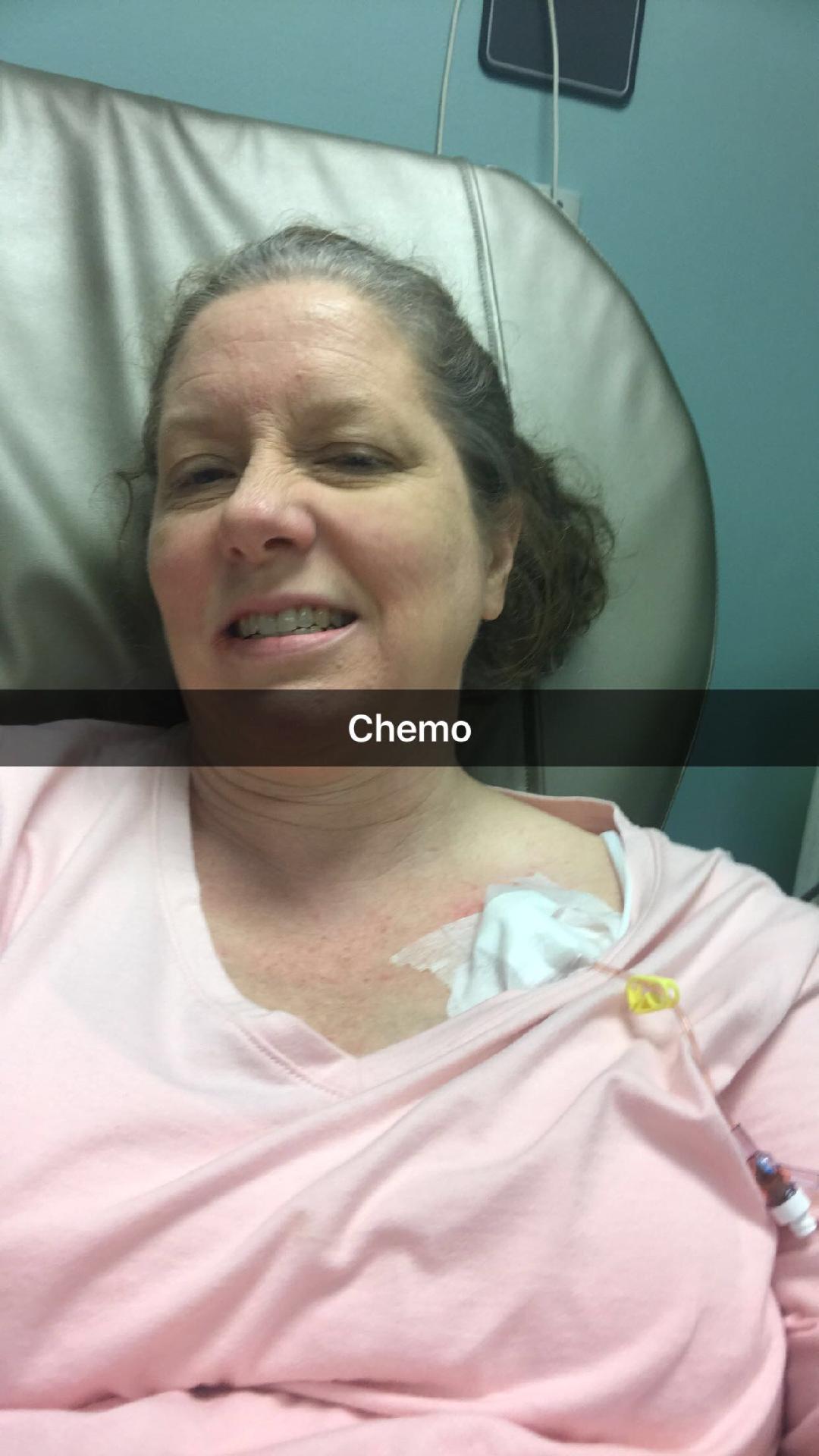
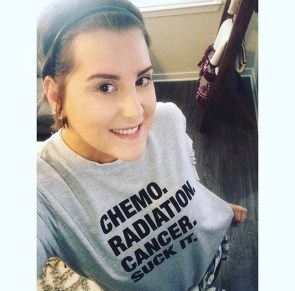
 January 19th I am out running errands at Target and get a call from Dr. White. “Hey Steff, I got your final path back, are you where you can talk?” yep I am at Target, go for it, “well it came back Stage 1, but all the hormone receptors are negative..” ok, what does that mean? “that means it is TRIPLE NEGATIVE BREAST CANCER, but we caught it early”. My world then changed and in the middle of the target line, I said “F#%&,, that means I have to do chemo”. So from that point on, slaying this tumor wasn’t going to be as easy as I thought. This was a game changer. The hardest part was telling my kiddo I had to do chemo now. For the first time I cried. It was just us, how was I going to do this. She can’t watch her mom wither away and die in a hospital bed. Luckily, she is a strong little warrior like myself and was up for the battle. Honestly, she was most bummed that our family sailing trip had to get postponed, but I mean who wouldn’t be bummed about that! So, January 25th I got my port placed for the chemo to get infused thru and my sentinel node biopsy, which came back negative yippee! Then on Wednesday February 1, I started chemo with my fabulous oncologist Dr. Gian. My besties Brooke and Jen from nursing school took me to my chemos and took such wonderful care of me. So many friends and family sent meals and gifts for us, it was truly a blessing. To all the random people out their who paid for groceries, ice cream, or meals while eating out, Thank you!
January 19th I am out running errands at Target and get a call from Dr. White. “Hey Steff, I got your final path back, are you where you can talk?” yep I am at Target, go for it, “well it came back Stage 1, but all the hormone receptors are negative..” ok, what does that mean? “that means it is TRIPLE NEGATIVE BREAST CANCER, but we caught it early”. My world then changed and in the middle of the target line, I said “F#%&,, that means I have to do chemo”. So from that point on, slaying this tumor wasn’t going to be as easy as I thought. This was a game changer. The hardest part was telling my kiddo I had to do chemo now. For the first time I cried. It was just us, how was I going to do this. She can’t watch her mom wither away and die in a hospital bed. Luckily, she is a strong little warrior like myself and was up for the battle. Honestly, she was most bummed that our family sailing trip had to get postponed, but I mean who wouldn’t be bummed about that! So, January 25th I got my port placed for the chemo to get infused thru and my sentinel node biopsy, which came back negative yippee! Then on Wednesday February 1, I started chemo with my fabulous oncologist Dr. Gian. My besties Brooke and Jen from nursing school took me to my chemos and took such wonderful care of me. So many friends and family sent meals and gifts for us, it was truly a blessing. To all the random people out their who paid for groceries, ice cream, or meals while eating out, Thank you!









 At that time I thought it was just a cyst from my cycle since I had one in the past but when it was still there in May I made an appointment with my Ob/Gyn. She said 90% of the lumps she sees are benign so I wasn’t too worried. She sent me for a diagnostic mammogram and ultrasound that same day. I didn’t think I would get any results that day so I went by myself…turns out that was a BIG mistake. When the radiologist came in after the tests I could tell by the look on his face that I should be worried. He told me I needed a biopsy because he couldn’t rule out cancer from what he saw and that I also had concerning calcifications in my other breast so he wanted me to have both breasts biopsied. While the radiologist did not have any bed-side manner, there was thankfully an ultrasound technician there who comforted me as I proceeded to have a panic attack.
At that time I thought it was just a cyst from my cycle since I had one in the past but when it was still there in May I made an appointment with my Ob/Gyn. She said 90% of the lumps she sees are benign so I wasn’t too worried. She sent me for a diagnostic mammogram and ultrasound that same day. I didn’t think I would get any results that day so I went by myself…turns out that was a BIG mistake. When the radiologist came in after the tests I could tell by the look on his face that I should be worried. He told me I needed a biopsy because he couldn’t rule out cancer from what he saw and that I also had concerning calcifications in my other breast so he wanted me to have both breasts biopsied. While the radiologist did not have any bed-side manner, there was thankfully an ultrasound technician there who comforted me as I proceeded to have a panic attack. Every prayer I sent up during this first scary month of unknowns was answered.
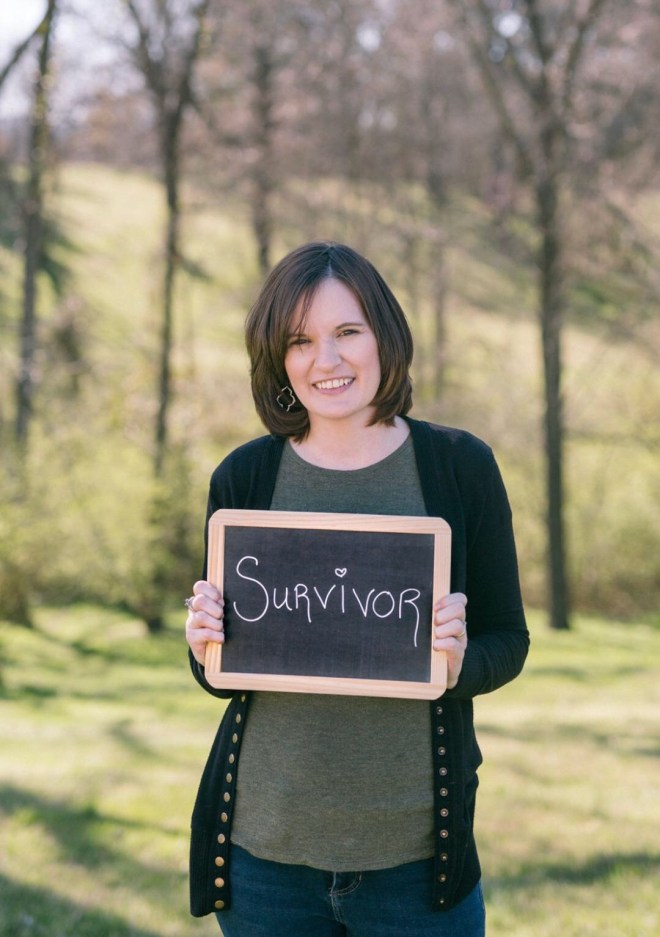
Every prayer I sent up during this first scary month of unknowns was answered.  surgeon had to go back in and take out more tissue. On December 18th I was finally cancer free!! Hearing those words after 7 months of hell was amazing! I give God all the glory for bringing me through this diagnosis. He answered every prayer I had.
surgeon had to go back in and take out more tissue. On December 18th I was finally cancer free!! Hearing those words after 7 months of hell was amazing! I give God all the glory for bringing me through this diagnosis. He answered every prayer I had.
































 feeling very tired from the pregnancy. I binge watched Impractical Jokers (I highly recommend!) and laughed a lot. Ted was always out on the phone calling doctors and friends to get opinions of doctors and who was the best. Sure enough we ended up with the BEST team of doctors who had a solid plan.
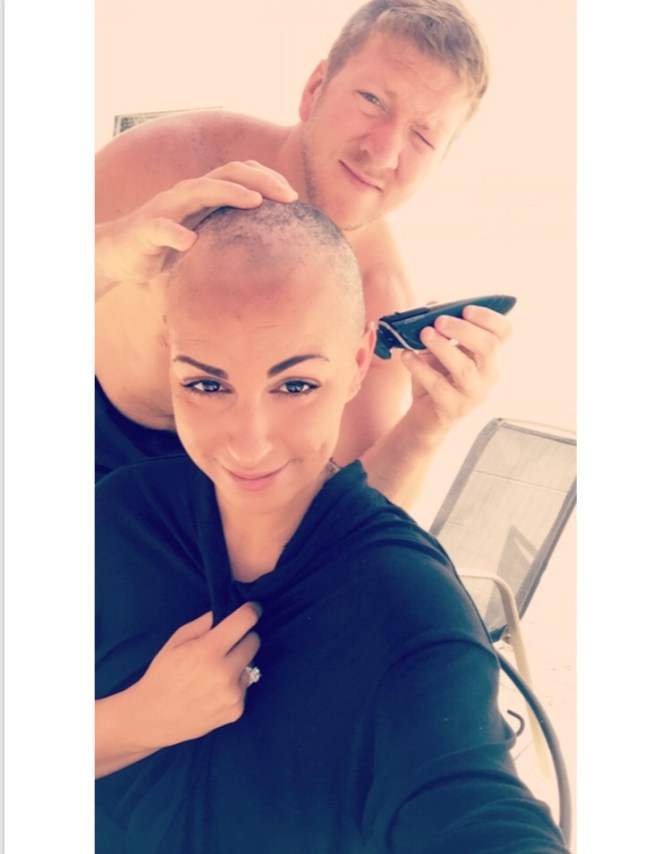
feeling very tired from the pregnancy. I binge watched Impractical Jokers (I highly recommend!) and laughed a lot. Ted was always out on the phone calling doctors and friends to get opinions of doctors and who was the best. Sure enough we ended up with the BEST team of doctors who had a solid plan. I did A/C first. Every three weeks instead of every two because my oncologist did not feel good about giving me the nuelasta shot (which brings up your white blood cells) while pregnant. My counts surprisingly all stayed very high during treatment until after I delivered, which just proves that Charlotte had my back and was fighting too! I am an artist so I brought some things to paint to help the time pass. I recommend bringing books, crosswords, painting supplies or whatever you enjoy doing. Thankfully I had very little side effects until the fourth and last A/C where I just got extremely tired. I did start to lose my hair after the second treatment. It was very itchy and hurt so I had my husband shave it. We got an amazing wig from HPI hair partners here in Nashville, TN and no one could tell It was a wig! People would always say how much they loved my haircut! We made it a funny experience since he is bald also, and it brought us that much closer together.
I did A/C first. Every three weeks instead of every two because my oncologist did not feel good about giving me the nuelasta shot (which brings up your white blood cells) while pregnant. My counts surprisingly all stayed very high during treatment until after I delivered, which just proves that Charlotte had my back and was fighting too! I am an artist so I brought some things to paint to help the time pass. I recommend bringing books, crosswords, painting supplies or whatever you enjoy doing. Thankfully I had very little side effects until the fourth and last A/C where I just got extremely tired. I did start to lose my hair after the second treatment. It was very itchy and hurt so I had my husband shave it. We got an amazing wig from HPI hair partners here in Nashville, TN and no one could tell It was a wig! People would always say how much they loved my haircut! We made it a funny experience since he is bald also, and it brought us that much closer together. Abramson suggested icing my fingers and toes. It is not fun. I REPEAT NOT FUN, but it is worth it because I have no neuropathy! I suggest wearing two pairs of latex gloves and two of the super fancy puke bags on your feet! I iced them for 1.5 hours every Tuesday for 9 Tuesdays. I am thankful for Vanderbilt 100 Oaks private infusion rooms so I could curse the ice without anyone knowing other than my husband and Jerry Seinfeld.
Abramson suggested icing my fingers and toes. It is not fun. I REPEAT NOT FUN, but it is worth it because I have no neuropathy! I suggest wearing two pairs of latex gloves and two of the super fancy puke bags on your feet! I iced them for 1.5 hours every Tuesday for 9 Tuesdays. I am thankful for Vanderbilt 100 Oaks private infusion rooms so I could curse the ice without anyone knowing other than my husband and Jerry Seinfeld.


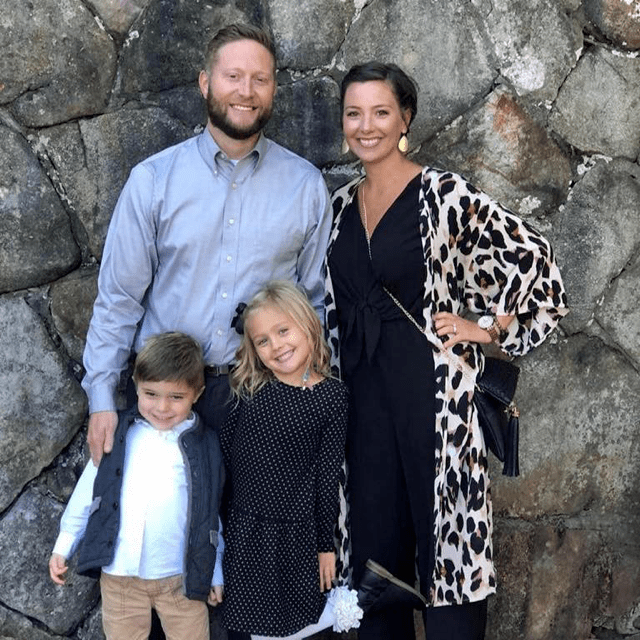
 surgery. Charlotte came home on December 18th and got to spend Christmas with us! It also meant that she got to come and celebrate with us at our last chemo treatment. There was no better feeling knowing that she got to be there by my side as I rang the bell, after all she fought too!
surgery. Charlotte came home on December 18th and got to spend Christmas with us! It also meant that she got to come and celebrate with us at our last chemo treatment. There was no better feeling knowing that she got to be there by my side as I rang the bell, after all she fought too!






 ensured I never had to go to an appointment alone no matter what resistance I gave. I now totally recommend having a note-taker in every appointment through the process, we had a notebook which we could use to do our homework after the appointments since 90% of what was happening did not get absorbed on the first pass. It wasn’t until months later when I reread all of my paperwork that I started to understand my diagnosis and all of the notes helped me greatly in sorting through the medical jargon.
ensured I never had to go to an appointment alone no matter what resistance I gave. I now totally recommend having a note-taker in every appointment through the process, we had a notebook which we could use to do our homework after the appointments since 90% of what was happening did not get absorbed on the first pass. It wasn’t until months later when I reread all of my paperwork that I started to understand my diagnosis and all of the notes helped me greatly in sorting through the medical jargon. leader as well as an incredible team who made the hardest days of my life possible. While my mom and friends and family showed up for my treatments and to sit with me on the hard days (the 2-4th days after the chemo), my work family kept me uplifted and feeling useful – albeit I wasn’t always able to do as much as I wanted. My first chemo treatment was the second week of January, 24 hours after having my chest port placed. I went through 6 rounds, 1 every 3 weeks, of the hard stuff which was then followed by 7 additional months of Herceptin to treat the Her2 positive diagnosis. I lost my hair, which I shaved before it fell out, and decided to go bald for the majority of the time…wigs just were not for me. One of the things that got me through chemo, aside from work, was staying active. I got a trainer to help me get my mobility back after the first surgery and then joined a fitness group. Staying busy was hugely beneficial for my recovery.
leader as well as an incredible team who made the hardest days of my life possible. While my mom and friends and family showed up for my treatments and to sit with me on the hard days (the 2-4th days after the chemo), my work family kept me uplifted and feeling useful – albeit I wasn’t always able to do as much as I wanted. My first chemo treatment was the second week of January, 24 hours after having my chest port placed. I went through 6 rounds, 1 every 3 weeks, of the hard stuff which was then followed by 7 additional months of Herceptin to treat the Her2 positive diagnosis. I lost my hair, which I shaved before it fell out, and decided to go bald for the majority of the time…wigs just were not for me. One of the things that got me through chemo, aside from work, was staying active. I got a trainer to help me get my mobility back after the first surgery and then joined a fitness group. Staying busy was hugely beneficial for my recovery. Once I finished chemotherapy I was able to get the second reconstructive surgery. This surgery, while hard to recover from due to the skin grafts of my new nipples, was a mental game changer – it helped me feel a bit more like myself. I was hesitant to have the reconstructive nipples, where the doctor makes nipples out of skin from another part of your body, but after strong recommendations I opted in and am today beyond thankful. While this isn’t for everyone, seeing myself look more similar to my “old self” helped me move forward and accept my new body.
Once I finished chemotherapy I was able to get the second reconstructive surgery. This surgery, while hard to recover from due to the skin grafts of my new nipples, was a mental game changer – it helped me feel a bit more like myself. I was hesitant to have the reconstructive nipples, where the doctor makes nipples out of skin from another part of your body, but after strong recommendations I opted in and am today beyond thankful. While this isn’t for everyone, seeing myself look more similar to my “old self” helped me move forward and accept my new body.
 Writing my story and sharing with friends and family was therapeutic in my process. My full journey and more about life beyond cancer can be found on my blog at
Writing my story and sharing with friends and family was therapeutic in my process. My full journey and more about life beyond cancer can be found on my blog at